How Long Must We Wait for a Corona Virus Cure?
The Limits of Science
The common cold is a viral infectious disease of the upper respiratory tract. Catching a cold is easy enough, and it can lead to health complications and death in extreme cases. It has been with humans since medical records have been kept. To date, there is no antiviral medication that is an effective cure for the Common Cold.
In 1983, scientists discovered the virus that causes of HIV (AIDS). Billions of dollars have been spent in R&D pursuing an effective vaccine and cure by the global scientific community. Since the beginning of its discovery, 74.9 million people have become infected with HIV and 32.0 million have died of AIDS-related illnesses. An estimated 1.7 million individuals worldwide acquired HIV in 2019, marking a 23% decline in new HIV infections since 2010.
Unlike COVID-19 which is airborne spread, the infectious spread of AIDS is limited to the fluid transmission of the disease from one infected person to another.
Like the Common Cold, no amount of money, time, scientific knowledge, technology and effort to date has so far produced a cure for AIDS.
Covid-19, a 21st century challenge for science
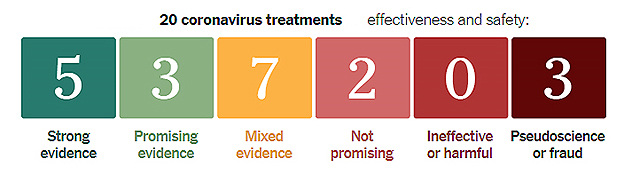
Doctors and scientists are scrambling to find treatments and drugs that can save the lives of infected people and perhaps even prevent infection. Politicians and a global economy is literally dying to get back to work.
Researchers around the world are developing more than 155 vaccines against the coronavirus, and 23 vaccines are in human trials. Vaccines typically require years of research and testing before reaching the clinic, but scientists are racing to produce a safe and effective vaccine by next year. 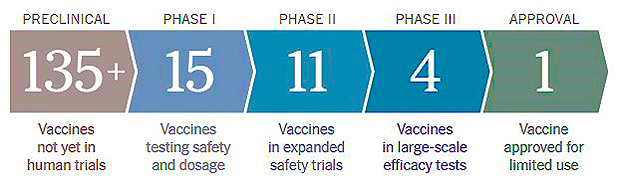
On 29 June, University of Oxford clinical scientists Martin Landray and Peter Horby changed how physicians around the world consider treating COVID-19—for the third time in little more than 3 weeks.
The principal investigators of a U.K. megatrial called Recovery, which has been testing existing drugs as therapies for the new infection, the pair had just finished reviewing data from 1596 patients who had received a combination of lopinavir and ritonavir, two antivirals known to curb HIV, and 3376 patients who had received only standard care. In a press release, they and their Recovery colleagues announced there had been no significant difference in the death rate between the two groups. “This could have worked. And it was a bust,” says Eric Topol, director of the Scripps Research Translational Institute.
Here’s what we know…
- Scientists around the world are working on potential treatments and vaccines for the new coronavirus disease known as COVID-19.
- Several companies are working on antiviral drugs, some of which are already in use against other illnesses, to treat people who already have COVID-19.
- Other companies are working on vaccines that could be used as a preventive measure against the disease.
With confirmed COVID-19 cases worldwide surpassing 14 million and continuing to grow, scientists are pushing forward with efforts to develop vaccines and treatments to slow the pandemic and lessen the disease’s damage. Some of the earliest treatments will likely be drugs that are already approved for other conditions, or have been tested on other viruses. Meaning, what we can expect are treatments, not a cure for the near term, if ever. We are still working on a cure for the common cold.
Today’s COVID-19 Medical Treatment Options, and Political Snake Oil
Treatments Expected to Block the Virus
Antivirals can stop viruses such as H.I.V. and hepatitis C from hijacking our cells. Scientists are searching for antivirals that work against the new coronavirus.
- STRONG EVIDENCE EMERGENCY USE AUTHORIZATION
Remdesivir
Remdesivir, made by Gilead Science, was the first drug to get emergency authorization from the F.D.A. for use on Covid-19. It stops viruses from replicating by inserting itself into new viral genes. Remdesivir was originally tested as an antiviral against Ebola and Hepatitis C, only to deliver lackluster results. But preliminary data from trials that began this spring suggested the drug can reduce the hospital stays of people with severe cases of Covid-19 from 15 to 11 days. These early results did not show any effect on mortality, though retrospective data released in July hints that the drug might reduce death rates among those who are very ill.
- TENTATIVE OR MIXED EVIDENCE
Favipiravir
Originally designed to beat back influenza, favipiravir blocks a virus’s ability to copy its genetic material. A small study in March indicated the drug might help purge the coronavirus from the airway, but results from larger, well-designed clinical trials are still pending.
EIDD-2801
Another antiviral originally designed to fight the flu, EIDD-2801 has had promising results against the new coronavirus in studies in cells and on animals. It is still being tested in humans.
Recombinant ACE-2
To enter cells, the coronavirus must first unlock them — a feat it accomplishes by latching onto a human protein called ACE-2. Scientists have created artificial ACE-2 proteins which might be able to act as decoys, luring the coronavirus away from vulnerable cells. Recombinant ACE-2 proteins have shown promising results in experiments on cells, but not yet in animals or people.
- NOT PROMISING
Lopinavir and ritonavir
Twenty years ago, the F.D.A. approved this combination of drugs to treat H.I.V. Recently, researchers tried them out on the new coronavirus and found that they stopped the virus from replicating. But clinical trials in patients proved disappointing. In early July, the World Health Organization suspended trials on patients hospitalized for Covid-19. But they didn’t rule out studies to see if the drugs could help patients not sick enough to be hospitalized, or to prevent people exposed to the new coronavirus from falling ill. The drug could also still have a role to play in certain combination treatments.
Hydroxychloroquine and chloroquine
German chemists synthesized chloroquine in the 1930s as a drug against malaria. A less toxic version, called hydroxychloroquine, was invented in 1946, and later was approved for other diseases such as lupus and rheumatoid arthritis.
At the start of the Covid-19 pandemic, researchers discovered that both drugs could stop the coronavirus from replicating in cells. Since then, they’ve had a tumultuous ride through the first few months of the pandemic. A few small studies on patients offered some hope that hydroxychloroquine could treat Covid-19. The World Health Organization launched a randomized clinical trial in March to see if it was indeed safe and effective for Covid-19, as did Novartis and a number of universities.
Meanwhile, President Trump repeatedly promoted hydroxychloroquine at press conferences, touting it as a “game changer,” and even took it himself. The F.D.A. temporarily granted hydroxychloroquine emergency authorization for use in Covid-19 patients — which a whistleblower later claimed was the result of political pressure. In the wake of the drug’s newfound publicity, demand spiked, resulting in shortages for people who rely on hydroxychloroquine as a treatment for other diseases.
When data emerged from the randomized clinical trials, the message was clear: hydroxychloroquine didn’t help people with Covid-19 get better or prevent healthy people from contracting the coronavirus. (One large-scale study that concluded the drug was harmful as well was later retracted.) The World Health Organization, the National Institutes of Health and Novartis have since halted trials investigating hydroxychloroquine as a treatment for Covid-19, and the F.D.A. revoked its emergency approval. The F.D.A. now warns that the drug can cause a host of serious side effects to the heart and other organs when used to treat Covid-19.
In July, researchers at Henry Ford hospital in Detroit published a study finding that hydroxychloroquine reduced mortality in Covid-19 patients. President Trump praised the study on Twitter, but experts raised doubts about it because it was not a randomized controlled trial. Still, the White House has initiated a push for the F.D.A. to reauthorize hydroxychloroquine as an emergency Covid-19 treatment.
Despite negative results, a number of hydroxychloroquine trials have continued. A recent analysis by STAT and Applied XL found more than 180 ongoing clinical trials testing hydroxychloroquine or chloroquine, for treating or preventing Covid-19. Although it’s clear the drugs are no panacea, it’s possible they could work in combination with other treatments, or when given in early stages of the disease.
Mimicking the Immune System
Most people who get Covid-19 successfully fight off the virus with a strong immune response. Drugs might help people who can’t mount an adequate defense.
- PROMISING EVIDENCE EMERGENCY USE AUTHORIZATION
Convalescent plasma
A century ago, doctors filtered plasma from the blood of recovered flu patients. So-called convalescent plasma, rich with antibodies, helped people sick with flu fight their illness. Now researchers are trying out this strategy on Covid-19. Early trials with convalescent plasma have yielded promising, if preliminary, results, and the F.D.A. has authorized its use on very sick patients infected by the coronavirus.
- TENTATIVE OR MIXED EVIDENCE
REGN-COV2 and other monoclonal antibodies
Convalescent plasma contains a mix of different antibodies, some of which can attack the coronavirus, and some of which can’t. Researchers have been sifting through the slurry for the most potent antibodies against Covid-19. Synthetic copies of these molecules, known as monoclonal antibodies, can be manufactured in bulk and then injected into patients. Safety trials for this treatment have only just begun, with several more on the way.
Interferons
Interferons are molecules our cells naturally produce in response to viruses, rousing the immune system to attack. Injecting synthetic interferons is now a standard treatment for a number of immune disorders. Rebif, for example, is prescribed for multiple sclerosis. Early studies, including experiments in mice and cells, hint that injecting interferons may help against Covid-19. There’s even some evidence that the molecules could help prevent healthy people from getting infected.
Putting Out Friendly Fire
The most severe symptoms of Covid-19 are the result of the immune system’s overreaction to the virus. Scientists are testing drugs that can rein in its attack
- STRONG EVIDENCE
Dexamethasone
This cheap and widely available steroid blunts many types of immune responses. Doctors have long used it to treat allergies, asthma and inflammation. In June, it became the first drug shown to reduce Covid-19 deaths. That study of more than 6,000 people, which has not yet been published in a scientific journal, found that dexamethasone reduced deaths by one-third in patients on ventilators, and by one-fifth in patients on oxygen. It may be less likely to help — and may even harm — patients who are at an earlier stage of Covid-19 infections, however. In its Covid-19 treatment guidelines, the National Institutes of Health recommends only using dexamethasone in patients with COVID-19 who are on a ventilator or are receiving supplemental oxygen.
- PROMISING EVIDENCE EMERGENCY USE AUTHORIZATION
Cytosorb
Cytosorb is a cartridge that filters immune-signalling molecules called cytokines from the blood. Although cytokines are essential for fighting off diseases, they can sometimes trigger a runaway response. The body produces so much inflammation that it damages itself. By removing excess cytokines, Cytosorb may be able to cool this so-called cytokine storm. The machine can purify a patient’s entire blood supply about 70 times in a 24-hour period. It was granted emergency use authorization by the F.D.A. for Covid-19 after reports in March suggested that it had helped dozens of severely ill Covid-19 patients in Europe and China. Many clinical trials evaluating the device’s effectiveness against Covid-19 are now underway.
- TENTATIVE OR MIXED EVIDENCE
Cytokine Inhibitors
Researchers have created a number of drugs that can potentially halt cytokine storms, and have proven effective against arthritis and other inflammatory disorders. Some turn off the supply of molecules that launch the production of the cytokines themselves. Others block the receptors on immune cells to which cytokines would normally bind. A few block the cellular messages they send. Against the coronavirus, several of these drugs, including tocilizumab, sarilumab and anakinra, have offered modest help in some trials, but faltered in others. The drug company Regeneron recently announced that a branded version of sarilumab, Kevzara, failed Phase 3 clinical trials.
Stem cells
Certain kinds of stem cells can secrete anti-inflammatory molecules. Over the years, researchers have tried to use them as a treatment for cytokine storms, and now dozens of clinical trials are under way to see if they can help patients with Covid-19. But these stem cell treatments haven’t worked well in the past, and it’s not clear yet if they’ll work against the coronavirus.
Assisting Our Bodies
Caregivers can physically adjust a patient’s body to help weather Covid-19.
- STRONG EVIDENCE
Prone positioning
The simple act of flipping Covid-19 patients onto their bellies opens up the lungs. The maneuver has become commonplace in hospitals around the world since the start of the pandemic. It might help some individuals avoid the need for ventilators entirely. The treatment’s benefits continue to be tested in a range of clinical trials.
- STRONG EVIDENCE EMERGENCY USE AUTHORIZATION
Ventilators and other respiratory support devices
Devices that help people breathe are an essential tool in the fight against deadly respiratory illnesses. Some patients do well if they get an extra supply of oxygen through the nose or via a mask connected to an oxygen machine. Patients in severe respiratory distress may need to have a ventilator breathe for them until their lungs heal. Doctors are divided about how long to treat patients with noninvasive oxygen before deciding whether or not they need a ventilator. Not all Covid-19 patients who go on ventilators survive, but the devices are thought to be lifesaving in many cases.
Undoing the Damage
Covid-19 can harm not just the lungs, but other parts of the body. Researchers are searching for ways to block or reverse this devastation.
Enoxaparin and other anticoagulants – The coronavirus can invade cells in the lining of blood vessels, leading to tiny clots that can cause strokes and other serious harm. Breaking up these clots with anticoagulants, which have long been used on patients with various heart conditions, improves the prospects of seriously ill patients. Early data has linked the use of anticoagulants to survival among Covid-19 patients, and many clinical trials teasing out this relationship are now underway.
- PROMISING EVIDENCE
Renal replacement therapy
About one in five people with Covid-19 who are admitted to the ICU suffer from acute kidney injury. It’s not clear yet why — possibilities include the coronavirus infecting kidney cells or the immune system attacking the kidneys with a cytokine storm. In its guidelines for treating Covid-19, the National Institutes recommends filtering toxins from the blood with dialysis or other forms of renal replacement therapy. But they warn that few studies have yet been carried out to determine the best treatment for damaged kidneys.
Pseudoscience and Fraud
False claims about Covid-19 cures abound. The F.D.A. maintains a list of more than 80 fraudulent Covid-19 products, and the W.H.O. debunks many myths about the disease.
WARNING: DO NOT DO THIS
Drinking or injecting bleach and disinfectants
In April, President Trump suggested that disinfectants such as alcohol or bleach might be effective against the coronavirus if directly injected into the body. His comments were immediately refuted by health professionals and researchers around the world — as well as the makers of Lysol and Clorox. Ingesting disinfectant would not only be ineffective against the virus, but also hazardous — possibly even deadly. In July, Federal prosecutors charged four Florida men with marketing bleach as a cure for COVID-19.
WARNING: NO EVIDENCE
UV light
President Trump also speculated about hitting the body with “ultraviolet or just very powerful light.” Researchers have used UV light to sterilize surfaces, including killing viruses, in carefully managed laboratories. But UV light would not be able to purge the virus from within a sick persons’ body. This kind of radiation can also damage the skin. Most skin cancers are a result of exposure to the UV rays naturally present in sunlight.
WARNING: NO EVIDENCE
Silver
The F.D.A. has threatened legal action against a host of people claiming silver-based products are safe and effective against Covid-19 — including televangelist Jim Bakker and InfoWars host Alex Jones. Several metals do have natural antimicrobial properties. But products made from them have not been shown to prevent or treat the coronavirus.
For more details on evaluating treatments, see the N.I.H. Covid-19 Treatment Guidelines.




Leave a Reply
Join the Community discussion now - your email address will not be published, remains secure and confidential. Mahalo.